
My name is Jorge Castillo and I am originally from Lima, Peru. I finished dental school at the Universidad Peruana Cayetano Heredia in Perú . My interest in Dentistry arose from my dad, who is a Pediatric Dentist, trained in the 60’s in Pediatric Dentistry at the Eastman Dental Center in Rochester, New York, with a brilliant career in Peru, both professionally and academically. Since I was a dental student, my favorite specialty was Pediatric Dentistry. Restoring dental health for children and enjoying when a child finished their dental appointment with a big smile, especially because I was an anxious patient when I was a child, were determining factors for me to choose pediatric dentistry as the specialty I wanted to follow. Also, during my years of dental school, I had the opportunity to treat various types of patients in various places: the dental clinic at the university, in the poorer areas of Lima, and in the remote communities of Peru. That reaffirmed my interest in doing good things for our children.

After finishing my dental degree, I was fortunate to begin graduate studies in Pediatric Dentistry at the University of Connecticut and do a Masters of Dental Sciences at the same University. The years at UConn were wonderful and I was lucky to have faculty such as Norman Tinanoff, Jim Crall, Andrew Poole among others. When I returned to Peru, I began my career as a faculty member in my dental school in Lima and working in private practice with my father and my sister.
A few years later, I was accepted to start an orthodontic program at the University of Washington. My training in Orthodontics was incredible and here I was also fortunate to have top faculty members such as Vince Kokich, Peter Shapiro, Greg King, Don Joondeph, Greg Huang among others. A requirement for the program to which I had applied, was to do a Master of Science in Science. Through Dr. Doug Ramsay, I had the honor of working with Dr. Peter Milgrom who was my mentor during those years. I had the opportunity to work with him in Public Health projects in the Department of Oral Health Sciences and in the Dental Fears Research Clinic. That experience was the one that finally shaped my interest in research and finding solutions to the oral health problems in children.

When I returned to Peru in 2000, my career was consolidated. I returned to private practice with my father, I began a new cycle of teaching in the postgraduate course of Pediatric Dentistry of the UPCH and I began to be invited to give courses and conferences in various cities in Peru, and many countries around the world. I have been fortunate to give courses and conferences in Argentina, Bolivia, Brazil, Colombia, Chile, Ecuador, Paraguay, Uruguay, Venezuela, Mexico, United States, Canada, Spain, Portugal, South Korea, United Arab Emirates, Taiwan, and Iran. Soon I will visit South Africa and India. In addition, I began to get involved with institutions beginning with the presidency of the Peruvian Society of Pediatric Dentistry and then of the Peruvian Society of Orthodontics.

My relationship with the UW held firm and I became an Affiliate Assistant Professor at the Department of Oral Health Sciences, a position I hold now. That opportunity led to many joint research projects between the University of Washington and the Peruvian University Cayetano Heredia, and the exchange of students and faculty between the two universities. One of the most important milestones was the organization of the Latin American Workshop on Clinical Research Methods in Oral Health, thanks to the leadership of Dr. Timothy DeRouen and Dr. Ana Lucia Seminario. This activity was held twice in Lima and the lectures were given by faculty members from the University of Washington. We received a large group of students from various parts of Peru and Latin America.
In addition to that, I started my international career as a board member of the International Association of Pediatric Dentistry. I was president of the IAPD from 2013 to 2015 and that was a wonderful opportunity, not only to meet people from all over the world but also to get to know the oral health situation of children globally. I am currently in a second term as president of the IAPD and we have very important plans to promote children’s oral health around the world.

Almost two years ago, I was diagnosed with Non-Hodgkins Lymphoma. For me it was a hard fight against the disease, but finally and after a few months of treatment I was able to succeed and now I am recovered and with all the strength to continue working hard. I want to thank everyone who was involved in my recovery. When you go through a difficult time in your life, like a did, you end up appreciating life and the people around you, much better.

There are so many plans for the future, in my professional and personal life. As a Member of the Board of Directors of the UW Timothy A. DeRouen Center for Global Oral Health, we will continue working with Dr Ana Lucia Seminario and the DeRouen Center with projects designed to improve oral health in our population. Thanks to the DeRouen Center for the opportunity to work together.











 I started a project which was new to me both in science and methodology. My project was about the innate immunity function of taste receptors relating to dental caries and periodontal disease in Thai dental patients. Learning new things and developing new skills were challenging. I’ve had struggled along the way. All the mentors in the program were very understanding and provided me with all their support to achieve my goal. I’ve learned academic and life skills from all the mentors. I feel that they work so hard in collaborating between countries/universities. Besides the curriculum, I feel thankful to have them devoting their time guiding me through the journey. I am ready to pay it forward and learn more to help improve dental public health.
I started a project which was new to me both in science and methodology. My project was about the innate immunity function of taste receptors relating to dental caries and periodontal disease in Thai dental patients. Learning new things and developing new skills were challenging. I’ve had struggled along the way. All the mentors in the program were very understanding and provided me with all their support to achieve my goal. I’ve learned academic and life skills from all the mentors. I feel that they work so hard in collaborating between countries/universities. Besides the curriculum, I feel thankful to have them devoting their time guiding me through the journey. I am ready to pay it forward and learn more to help improve dental public health.


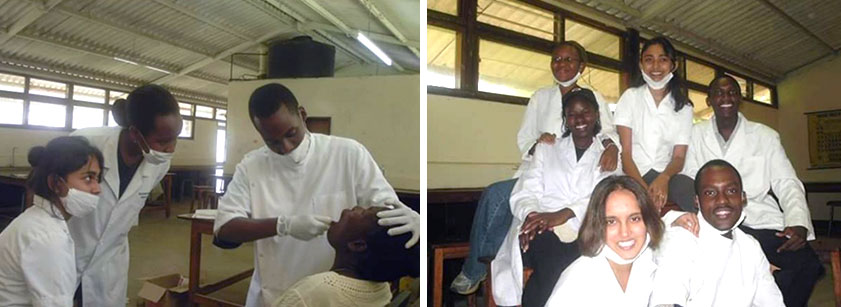
 The decision to further my education opened a new window of opportunities for me. It is during this period that I appreciated the importance of research and the impact of HIV/AIDS on oral health. By taking care of HIV infected children, I began to understand the health, social and economic struggles associated with HIV infection. It is also during this time that I met Dr. Arthur Kemoli (University of Nairobi). Through him and Dr. Ana Lucia Seminario (University of Washington), I received funding from International Association for Dental Research (IADR) that enabled me to attend the Summer Institute in Clinical Dental Research in the University of Washington. This was a wonderful opportunity which not only whet my appetite for research, but also exposed me to a new mentor, Dr. Ana Lucia Seminario. Immediately after I got home from the Summer Institute, I was able to write a research proposal, get ethical review and start data collection on oral health status of under five-year-old children in Kisumu County primary schools. Unfortunately, this activity was disrupted by the COVID-19 pandemic. I look forward to continuing with data collection once the disease is controlled.
The decision to further my education opened a new window of opportunities for me. It is during this period that I appreciated the importance of research and the impact of HIV/AIDS on oral health. By taking care of HIV infected children, I began to understand the health, social and economic struggles associated with HIV infection. It is also during this time that I met Dr. Arthur Kemoli (University of Nairobi). Through him and Dr. Ana Lucia Seminario (University of Washington), I received funding from International Association for Dental Research (IADR) that enabled me to attend the Summer Institute in Clinical Dental Research in the University of Washington. This was a wonderful opportunity which not only whet my appetite for research, but also exposed me to a new mentor, Dr. Ana Lucia Seminario. Immediately after I got home from the Summer Institute, I was able to write a research proposal, get ethical review and start data collection on oral health status of under five-year-old children in Kisumu County primary schools. Unfortunately, this activity was disrupted by the COVID-19 pandemic. I look forward to continuing with data collection once the disease is controlled. I am Yan Wang. I was born in China with a great passion for numbers. My undergraduate major is Mathematics, with a double major in Computer Science. I received my PhD in Biostatistics of School of Public Health at UCLA in 2019. My research passion is the joint research of HIV and oral health.
I am Yan Wang. I was born in China with a great passion for numbers. My undergraduate major is Mathematics, with a double major in Computer Science. I received my PhD in Biostatistics of School of Public Health at UCLA in 2019. My research passion is the joint research of HIV and oral health.  My passion in HIV/AIDS research started from a multi-site adherence collaboration in HIV across sixteen studies from fourteen universities and institutions. With the opportunity to collaborated with all world well-known scientists, I was responsible for coordinating the data transfer, data management, statistical analysis as well as modeling and publications. We used Medication Event Monitoring System (MEMS®) to record the date and time medication events. In the later project, we used Wisepill® box (designed by a South African company), and then Ingestible Sensor (Proteus) to measure HIV adherence in real-time, together with customized text messages. It was very challenging to have optimal adherence lifetime, as it is hard to maintain the optimal adherence.
My passion in HIV/AIDS research started from a multi-site adherence collaboration in HIV across sixteen studies from fourteen universities and institutions. With the opportunity to collaborated with all world well-known scientists, I was responsible for coordinating the data transfer, data management, statistical analysis as well as modeling and publications. We used Medication Event Monitoring System (MEMS®) to record the date and time medication events. In the later project, we used Wisepill® box (designed by a South African company), and then Ingestible Sensor (Proteus) to measure HIV adherence in real-time, together with customized text messages. It was very challenging to have optimal adherence lifetime, as it is hard to maintain the optimal adherence. 
 I received my T37 GATHER (Global Alliance for Training in Health Equity Research) fellowship in 2019. This fellowship supported my research in African Population Health Research Center (APHRC) in Nairobi, Kenya. I made a lot of friends with the researchers in Kenya. During that time, I learned of the work of both Drs. Ana Lucia Seminario and Arthur Kemoli. I joint their research team on the CHOMP (Children’s Healthy Oral Management Project) among HIV-infected children, the oral health of refugee children Washington State, and the infant oral mutilation traditional practice in East Africa. Since then, we have started an ongoing collaboration. After my GATHER training, I received my T32 UCLA postdoctoral fellowship in 2020, focused on Global AIDS prevention. I joint Dr. Grace Aldrovandi’s research team in 2020. I was very fortunate to participate in the COVID study of high-risk health services workers at UCLA and first responders in the Los Angeles County Fire Department. We compared the humoral responses to mRNA vaccine by prior infection and by vaccine type.
I received my T37 GATHER (Global Alliance for Training in Health Equity Research) fellowship in 2019. This fellowship supported my research in African Population Health Research Center (APHRC) in Nairobi, Kenya. I made a lot of friends with the researchers in Kenya. During that time, I learned of the work of both Drs. Ana Lucia Seminario and Arthur Kemoli. I joint their research team on the CHOMP (Children’s Healthy Oral Management Project) among HIV-infected children, the oral health of refugee children Washington State, and the infant oral mutilation traditional practice in East Africa. Since then, we have started an ongoing collaboration. After my GATHER training, I received my T32 UCLA postdoctoral fellowship in 2020, focused on Global AIDS prevention. I joint Dr. Grace Aldrovandi’s research team in 2020. I was very fortunate to participate in the COVID study of high-risk health services workers at UCLA and first responders in the Los Angeles County Fire Department. We compared the humoral responses to mRNA vaccine by prior infection and by vaccine type.




