

Hello, my name is Brenda Okumu from Kenya. I graduated with a Bachelors in Dental Surgery from the University of Nairobi and later pursued a Masters in Dental Primary and Public Health at the University of Western Australia. My passion is in oral health promotion and research. Recently I have been a beneficiary of a thesis publishing program, a partnership between the University of Washington and University of Nairobi. Sitting at the experienced feet of Prof Ana Lucia Seminario and Prof Arthur Kemoli has been a great eye opener into world-class research and publishing. For the last 10 years I have been teaching at the School of Dentistry, Moi University. Currently I am at the department of Community, Preventive Dentistry and Periodontology, and have been the outreach coordinator since 2016.
Doing outreach is not only our co-operate social responsibility as an institution but also a key strategy in eliminating and preventing the impact of oral disease particularly among high risk, resource limited populations. We mainly target health schools in slum areas and children’s homes within Eldoret town and its environs for oral health education, free dental check-up, and basic treatment such as extraction. For comprehensive management we refer the patients to our facility at the school for subsidized or free treatment. Although the main participants are our faculty and students, over the years we have often partnered with visiting Indiana University dental faculty and students. It is through this partnership that to a large extent we have been able to sustain most of the activities, including offering free or subsidized treatment at the school. We also partner with Moi Teaching and Referral Hospital and Colgate Palmolive Limited, who have often provided manpower, materials and donations of free toothpaste and toothbrushes respectively.

Unfortunately, for the last one and half years we have not had any outreach events due to the Covid -19 situation. The risk for infection, coupled with the increased costs to carter for the extra personal protective equipment required are some of the challenges that compelled us to put the activities on hold. There is need to strategize on how we can carry on despite the pandemic which, it seems, may be here with us for much longer than we anticipated. Oral health is a key component of general health, and efforts towards primary health care in communities with limited or no access to dental services must not be delayed any longer if we are to sustain the gains that we have already made. Perhaps it is time to engage all the stakeholders in these discussions to allow for new policies on outreach activities and to seek out new partnerships that will support this course.

 I’m a former teacher, administrator, and have worked in education reform and to improve early learning systems and programs. So how did I get involved in oral health and spend ten years and counting doing this work? The story is long, but the reason is simple: I’m passionate about doing mission driven work, specifically social justice work, and oral health is a social justice and equity issue. Through my travels abroad, and my professional and personal experiences right here in Washington, I’ve seen how some people – particularly those with resources – have fantastic oral health and think very little about it, while others – often those with few resources – struggle to access even basic dental care and think about oral health constantly because they suffer with oral disease with no respite.
I’m a former teacher, administrator, and have worked in education reform and to improve early learning systems and programs. So how did I get involved in oral health and spend ten years and counting doing this work? The story is long, but the reason is simple: I’m passionate about doing mission driven work, specifically social justice work, and oral health is a social justice and equity issue. Through my travels abroad, and my professional and personal experiences right here in Washington, I’ve seen how some people – particularly those with resources – have fantastic oral health and think very little about it, while others – often those with few resources – struggle to access even basic dental care and think about oral health constantly because they suffer with oral disease with no respite.





 Hello, my name is Mink Lee, and I’m currently serving as an intern at the DeRouen Center for Global Oral Health at University of Washington. I work part-time as a registered dental hygienist and am also a graduate student pursuing a master’s degree in Public Health from California State University – Northridge (CSUN).
Hello, my name is Mink Lee, and I’m currently serving as an intern at the DeRouen Center for Global Oral Health at University of Washington. I work part-time as a registered dental hygienist and am also a graduate student pursuing a master’s degree in Public Health from California State University – Northridge (CSUN).


 My name is Jennifer N. Ricaldi-Camahuali, faculty in the Department of Social Dentistry at Cayetano Heredia Peruvian University (UPCH) in Peru. I have a specialty in Pediatric Dentistry and training in Clinical Epidemiology, and five years ago I came to Seattle and received a Master of Public Health in Global Health at the University of Washington (UW).
My name is Jennifer N. Ricaldi-Camahuali, faculty in the Department of Social Dentistry at Cayetano Heredia Peruvian University (UPCH) in Peru. I have a specialty in Pediatric Dentistry and training in Clinical Epidemiology, and five years ago I came to Seattle and received a Master of Public Health in Global Health at the University of Washington (UW). Hi, my name is Kemporn “Pom” Kitsahawong, I am a full-time pediatric dentist and Associate Professor in the Faculty of Dentistry, Khon Kaen University. I was one of the long-term (PhD) trainees in the Fogarty International Center Training Program in Clinical, Public Health and Behavioral Oral Health Research for Thailand under the collaboration between KKU and the University of Washington (UW). Through the generous support from NIH, I received the opportunity to attend the 2010 UW Summer Institute and subsequently enrolled in several epidemiology and biostatistics courses offered at the UW School of Dentistry during my first year in PhD in Oral Science program at KKU.
Hi, my name is Kemporn “Pom” Kitsahawong, I am a full-time pediatric dentist and Associate Professor in the Faculty of Dentistry, Khon Kaen University. I was one of the long-term (PhD) trainees in the Fogarty International Center Training Program in Clinical, Public Health and Behavioral Oral Health Research for Thailand under the collaboration between KKU and the University of Washington (UW). Through the generous support from NIH, I received the opportunity to attend the 2010 UW Summer Institute and subsequently enrolled in several epidemiology and biostatistics courses offered at the UW School of Dentistry during my first year in PhD in Oral Science program at KKU. Over the past 10 years after my training with the UW team, I have been assisting Dean Pitiphat in expanding the knowledge and expertise in clinical oral health research to LMIC’s in Asia. The International Workshops on “Clinical Research Methods in Oral Health” jointly organized by University of Washington, Thammasat University and Khon Kaen University was conducted every 2 years. In the recent workshops, I served as a mentor facilitating the trainees from the leading institutes in Southeast Asia countries on developing a research proposal. This was a great opportunity to be able to share the experience with several international participants and to build partnerships that have mutual benefits in this region. Regarding research support, I have received consecutive grants from KKU Research Unit, KKU Faculty of Dentistry and the Office of National Higher Education Science Research and Innovation Policy Council (NXPO). These allow my team to carry on our research and recruit additional junior clinicians into the team.
Over the past 10 years after my training with the UW team, I have been assisting Dean Pitiphat in expanding the knowledge and expertise in clinical oral health research to LMIC’s in Asia. The International Workshops on “Clinical Research Methods in Oral Health” jointly organized by University of Washington, Thammasat University and Khon Kaen University was conducted every 2 years. In the recent workshops, I served as a mentor facilitating the trainees from the leading institutes in Southeast Asia countries on developing a research proposal. This was a great opportunity to be able to share the experience with several international participants and to build partnerships that have mutual benefits in this region. Regarding research support, I have received consecutive grants from KKU Research Unit, KKU Faculty of Dentistry and the Office of National Higher Education Science Research and Innovation Policy Council (NXPO). These allow my team to carry on our research and recruit additional junior clinicians into the team.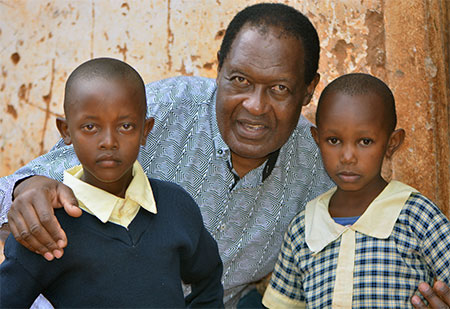

 Hi, my name is Janella Bermúdez and I’m currently a fourth-year dental student at the University of Washington. I am one of eight students selected to be in the Regional Initiatives in Dental Education (RIDE) Program, an educational track of the UW. Through community-based experiences, RIDE develops socially responsible dentists who foster a commitment to improving the oral health of vulnerable communities.
Hi, my name is Janella Bermúdez and I’m currently a fourth-year dental student at the University of Washington. I am one of eight students selected to be in the Regional Initiatives in Dental Education (RIDE) Program, an educational track of the UW. Through community-based experiences, RIDE develops socially responsible dentists who foster a commitment to improving the oral health of vulnerable communities. Joining the DeRouen Center
Joining the DeRouen Center